Describe the Process for Preauthorization for a Patient
This process allows for the greatest amount of a health plans resources to do the most good. In fact 75 of physicians participating in an AMA survey reported that issues related to the prior authorization process can cause patients to abandon their recommended course of treatment.
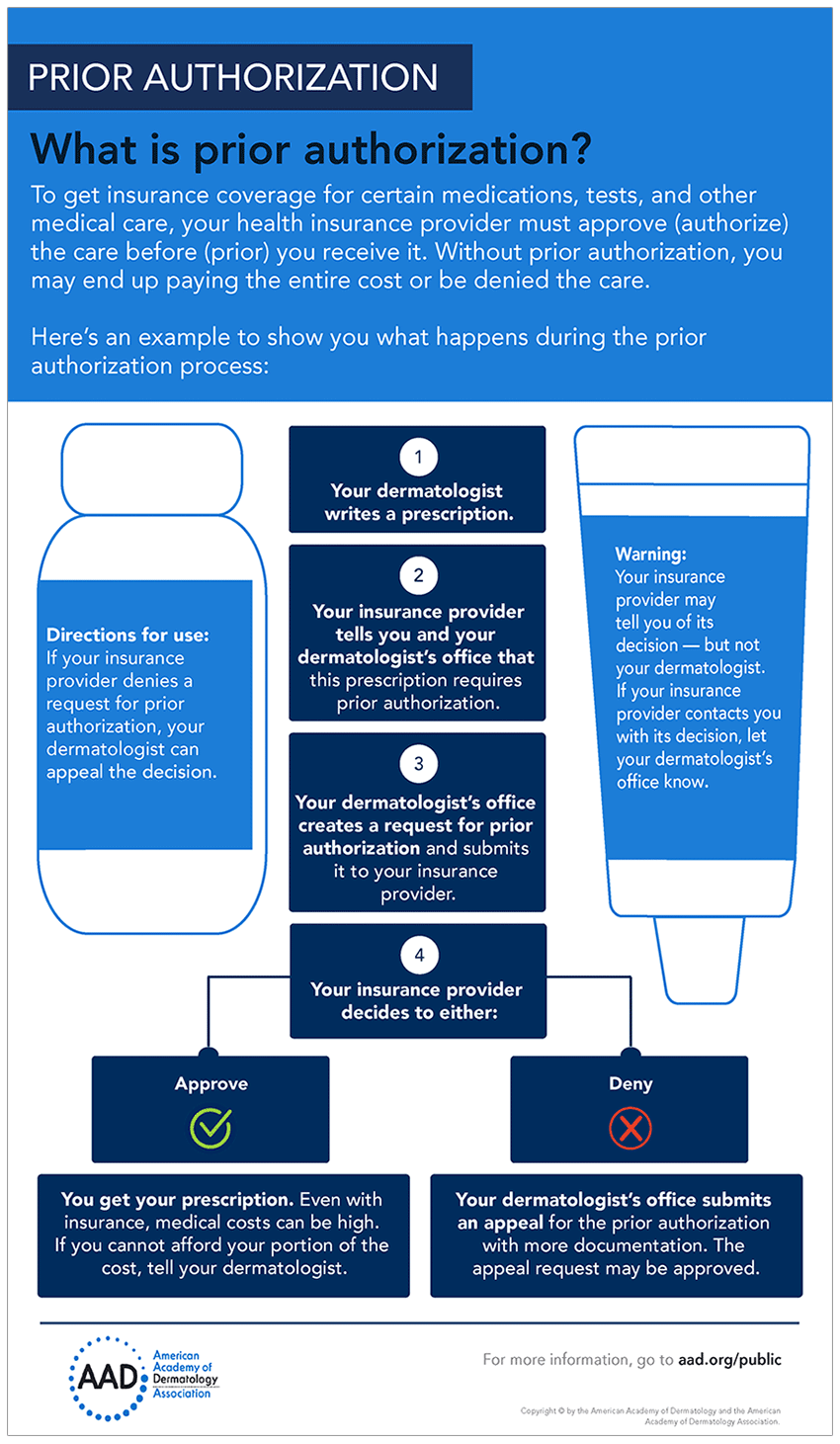
How To Get Prior Authorization For Medical Care
Verify insurance benefits determine whether the patients insurance covers the proposed service.
. The MA will need to gather the Patient health record prior authorization precertification request form copy of patients health insurance ID card a pen. Verification of eligibility for services b. A medically required health care service.
Verify eligibility status whether the patient has health insurance and will receive health insurance benefits. Ensure Seamless Preauthorization. Proofread the completed form and make any revisions needed.
Right handling of CPT codes is vital. Prior authorizationsometimes called precertification or prior approvalis a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. Gather the health record precertificationprior authorization request form copy of the health insurance ID card and a pen.
Understanding the Pre-authorization Process What is Pre-authorization. The second part of pre-certification is the reply from the payer which will tell the provider whether the service is covered. Constant communication between the provider and payer is crucial.
Normally a payer that authorizes a service prior to an encounter assigns an authorization number that you. In that same survey 28 of physicians reported that preauthorization has led to a serious adverse event for a patient in their care. VIIIC3b Define a patient-centered medical home service.
Sometimes called prior authorization prior approval or precertification. Fulfill the insurance carriers requirements for notifying the insurance carrier and obtaining authorization to provide the service. Insurance verification process is crucial for all encounters whether inpatient outpatient or ambulatory care.
Please list the payers you work with that require preauthorization for sleep testing briefly describe their preauthorization process and indicate the percentage of your patient population impacted by the payers policy. The AMA offers prior authorization resources to support reform improve practice efficiency and provide data to highlight the need for change. Individuals addresses all the tasks that are completed by administrative staff members during the medical billing process.
PA is a health plan utilization-management or cost-control process that requires physicians to obtain approval before a prescribed treatment test or medical service qualifies for payment. The person who handles billing entry has to select the correct current procedural. Your policy also states certain.
Everyone can agree that preauthorization in healthcare is the process of obtaining advance approval of a treatment plan proposed by a medical professional. Explain why and describe the process. The patients condition worsened resulting in the need for a prolonged hospitalization and an infusion of a costly drug infliximab infusion to.
It is a notification sent to a payer informing the payer that the patient wants to have a service completed. Outline managed care requirements for patient referral 3. VIIIC3c Prior to discharge the patient needs precertification for home health services.
So it is crucial to have the precertification sent either via phone email fax or an electronic transaction prior to services being provided to Mr. A precertification is the process where a patient is preapproved for coverage for a specific medical procedure. A decision by your health insurer or plan that a health care service treatment plan prescription drug or durable medical equipment is medically necessary.
Complete the PrecertificationPrior Authorization Request form using a pen. 1 Most commonly preauthorization and precertification refer to the process by which a patient is pre-approved for coverage of a specific medical procedure or prescription drug. Tap card to see definition.
As a medical billing professional dealing with prior authorization is a necessary part of the job. Prior authorization also known as preauthorization is the process of getting an agreement from the payer to cover specific services before the service is performed. Health insurance companies may require that patients.
These are terms that are often used interchangeably but which may also refer to specific processes in a health insurance or healthcare context. Primary Care Physician PCP Click card to see definition. It will ensure that the hospitalmedical office receives payment for services rendered and will help determine the.
Sometimes called prior authorization prior approval or precertification. Requires Preauth for OCST only or for all Testing. File the document in the health record after it.
Insurance eligibility verification and prior authorization is the first and vital step in the medical billing process. VIIIC4 Describe and identify the difference between fraud and abuse. Payer Preauth is submitted online by phone or by fax.
What is the process for obtaining precertification for these services. Pre -authorization is a process by which an Insured Person obtains written approval for certain medical procedures or treatments from GBGTieCare International prior to the commencement of the proposed medical treatment. File the document in the health record after it is faxed to the insurance carrier.
28 The percentage of physicians who say the prior authorization process has resulted in a serious adverse event for their patients eg death hospitalization disabilitypermanent bodily damage or other life-threatening event. Your health insurance or plan may require preauthorization for certain services before you receive them except in an emergency. Preauthorization also called prior authorization prior approval or precertification is how your health insurer decides if a service treatment plan or prescription drug is necessary.
If the precertification is not done charges are usually not covered. Healthcaregov defines medical preauthorization as a decision by your health insurer or plan that a health care service treatment plan prescription drug or durable medical equipment is medically necessary. Managed care plans including HMOs PPOs and EPOs require preauthorization for medical services such as surgery expensive medical tests and medication therapy.
Define a patient-centered medical home PCMH 5. In PPO plans PCP are the gatekeepers determine the appropiatnes for medical services. Preauthorization may be requested by calling the health insurance plan which should be documented in the patients electronic health record EHR.
The disagreement begins when deciding whether preauthorization is about providing patients with the best possible quality of care or reducing healthcare costs. The prior authorization PA hurdle led to a 5-day delay before the patient could start treatment the authors write. Proofread the completed form and make any revisions needed.
86 The percentage of physicians who describe prior authorization burdens as high or extremely high. The provider should ensure constant communication.

Importance Of Preauthorization In Revenue Cycle Management Rcm

Importance Of Preauthorization In Revenue Cycle Management Rcm

Front Line Stories How Today S Prior Authorization Processes Create A Burden Of Waste For Providers
Comments
Post a Comment